Unpacking the Ethical Dilemmas of CRISPR Technology in Genetic Disorder Treatment to CRISPR Technology
CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats) technology has revolutionized the field of genetic engineering, offering unprecedented precision and efficiency in editing genes. This breakthrough, discovered by scientists Jennifer Doudna and Emmanuelle Charpentier in 2012, has opened up new avenues for treating genetic diseases, but it also raises significant ethical concerns[1][2][3].
How CRISPR Works
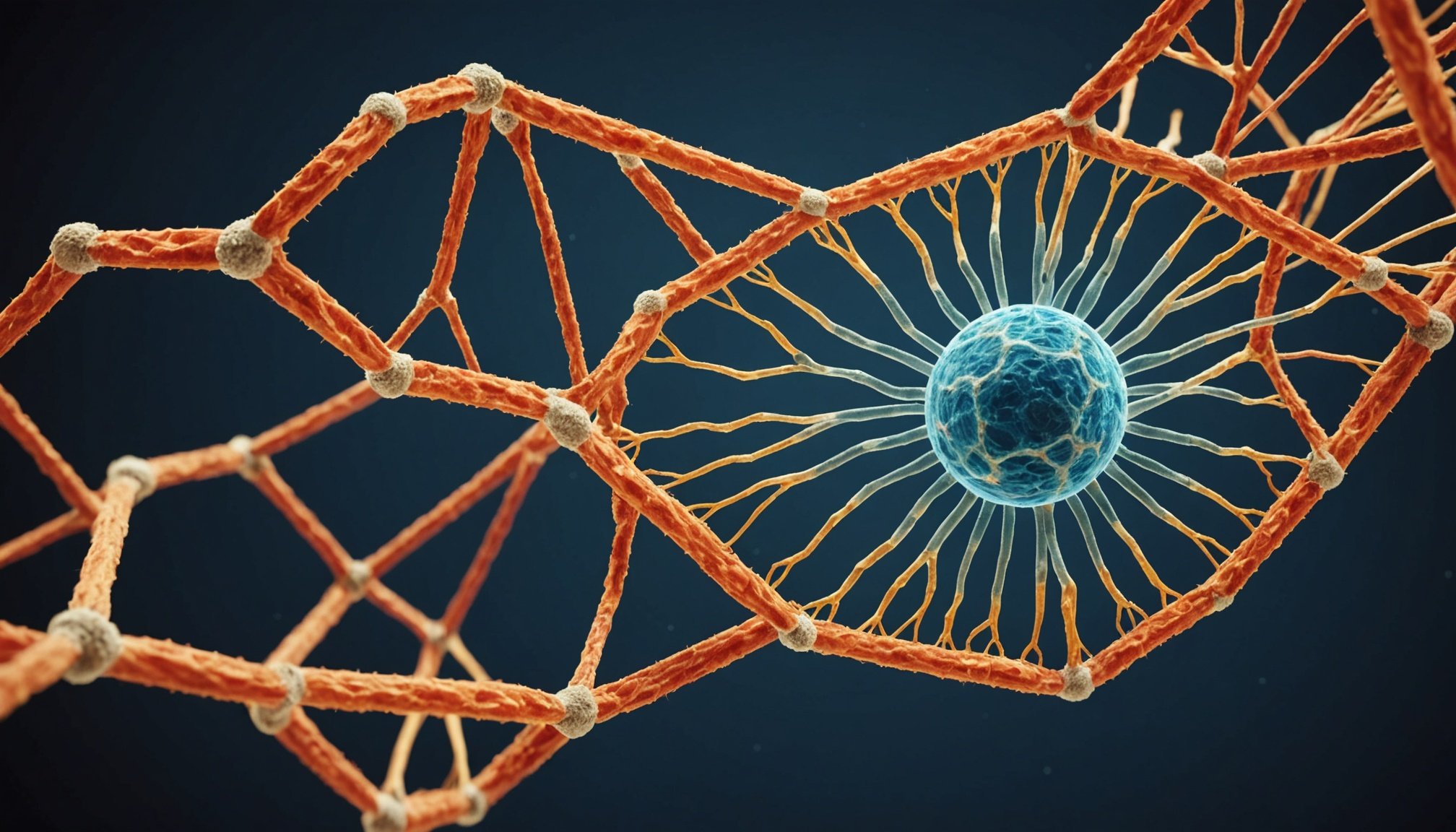
To understand the ethical dilemmas surrounding CRISPR, it’s essential to grasp how the technology functions. CRISPR uses a guide RNA to locate a specific DNA sequence and then employs an enzyme, typically Cas9, to cut the DNA at that site. This cut triggers the cell’s natural repair mechanisms, allowing researchers to edit the gene by inserting, deleting, or replacing DNA sequences. The precision of CRISPR-Cas9 is based on the Watson-Crick base-pairing rules, making it highly specific and versatile[1][2][3].
Also read : Unveiling the long-term effects of distance running on joint health: a comprehensive analysis
Applications in Genetic Disorder Treatment
CRISPR technology has shown immense promise in treating genetic diseases. Here are some key applications:
Treating Genetic Diseases
- Sickle Cell Disease and Beta-Thalassemia: The first CRISPR-based treatment, Casgevy, was approved by the FDA in 2023 for treating these blood disorders. It involves editing stem cells to disrupt a gene that represses normal hemoglobin production[1].
- Leber Congenital Amaurosis: CRISPR has been used to treat this inherited vision impairment by correcting the genetic mutation responsible for the disease[1][2].
- Cancer: CRISPR can enhance the body’s immune cells to target and eliminate cancer cells, and it can also be used to modify the tumor microenvironment[3].
Other Medical Applications
- AIDS: CRISPR can target and remove HIV DNA from patient cells, offering a potential cure for the disease[2].
- Genetic Engineering: CRISPR is used in various forms of genetic engineering, including the creation of chimeric antigen receptor T-cell (CAR-T cell) therapies and oncolytic viruses[3].
Ethical Issues Surrounding CRISPR
While CRISPR holds great potential for medical advancements, it also raises several ethical concerns.
Also to discover : Beginner”s roadmap: effortlessly embrace a plant-based lifestyle with these key tips
Germline Editing
One of the most contentious issues is the use of CRISPR for germline editing, which involves modifying DNA in human embryos, sperm, or eggs. This can lead to permanent changes in the human genome that are passed on to future generations. Critics argue that this could be used to create “designer babies” with enhanced traits, raising questions about the morality of tampering with human development and the potential for unequal access to such technology[1][2][4].
Off-Target Effects
CRISPR is not without its technical limitations. One significant concern is the risk of off-target effects, where the Cas enzyme cuts unintended parts of the genome, leading to unintended mutations. This can have serious consequences, especially in therapeutic applications where precision is crucial[3].
Access and Equity
The cost and accessibility of CRISPR-based therapies are also ethical concerns. For instance, the treatment Casgevy is costly and requires intensive medical procedures, making it inaccessible to many patients. This raises questions about equity and who will benefit from these advancements[1].
Public Perception and Regulation
Public sentiment and regulatory frameworks play a critical role in the ethical use of CRISPR. There is a need for clear guidelines and regulations to ensure that CRISPR technology is used responsibly. Scientists like Jennifer Doudna have called for a moratorium on human germline genome editing until the technology is better understood and ethical guidelines are in place[2][5].
Detailed Ethical Considerations
Here are some detailed ethical considerations surrounding the use of CRISPR technology:
Ethical Concerns in Human Embryos
- Designer Babies: The possibility of using CRISPR to enhance human traits such as intelligence, appearance, or athletic ability is a highly debated topic. It raises questions about the morality of such interventions and the potential for societal inequality[1][2][4].
- Unintended Consequences: Editing human embryos could introduce genetic errors that might not be immediately apparent but could have significant health implications for the individual and future generations[1][2].
Ethical Frameworks and Regulations
- Global Consensus: There is a need for a global consensus on the ethical use of CRISPR. Different countries have varying regulations, and a unified approach would help in ensuring responsible use[2][5].
- Public Education: Educating the public about the benefits and risks of CRISPR is crucial. This can help in building trust and ensuring that the technology is used in a way that is acceptable to society[2].
Balancing Benefits and Risks
- Therapeutic Benefits: CRISPR offers significant therapeutic benefits, especially for genetic diseases that have no current cure. However, these benefits must be weighed against the potential risks and ethical concerns[1][2][3].
- Risk Mitigation: Researchers are working on improving the precision of CRISPR to minimize off-target effects. Techniques such as using CRISPR nickases and paired nickases are being explored to enhance accuracy[3].
Practical Insights and Actionable Advice
Here are some practical insights and actionable advice for navigating the ethical dilemmas of CRISPR technology:
Ensuring Responsible Use
- Establish Clear Guidelines: Regulatory bodies should establish clear guidelines for the use of CRISPR in human therapy. This includes setting standards for safety, efficacy, and ethical considerations[2][5].
- Public Engagement: Scientists and policymakers should engage with the public to discuss the implications of CRISPR technology. This can help in building a consensus on its use and ensuring that it aligns with societal values[2].
Addressing Technical Limitations
- Improving Precision: Continuous research is needed to improve the precision of CRISPR technology. This includes developing new Cas proteins and editing strategies that minimize off-target effects[3].
- Clinical Trials: Rigorous clinical trials are essential to ensure the safety and efficacy of CRISPR-based therapies. These trials should be transparent and subject to strict regulatory oversight[1][3].
Examples and Anecdotes
The Case of He Jiankui
In 2018, Chinese scientist He Jiankui sparked global controversy by announcing the birth of the world’s first gene-edited human babies. He used CRISPR to edit the CCR5 gene in embryos to make them resistant to HIV. This move was widely criticized due to the lack of transparency, the risks involved, and the ethical implications of such a procedure[1][2].
Success Stories in Genetic Diseases
On the other hand, there have been several success stories where CRISPR has been used to treat genetic diseases. For example, CRISPR has been used to treat patients with sickle cell disease and Leber congenital amaurosis, offering new hope for patients with these debilitating conditions[1][2].
CRISPR technology is a double-edged sword, offering immense potential for treating genetic diseases but also raising significant ethical concerns. As we move forward, it is crucial to address these ethical dilemmas through rigorous research, clear regulatory frameworks, and public engagement.
Key Takeaways
- Precision and Safety: Ensuring the precision and safety of CRISPR technology is paramount. This includes minimizing off-target effects and conducting thorough clinical trials.
- Ethical Guidelines: Establishing and adhering to ethical guidelines is essential. This involves a global consensus on the use of CRISPR in human therapy and germline editing.
- Public Education: Educating the public about the benefits and risks of CRISPR can help in building trust and ensuring responsible use.
Table: Comparison of CRISPR with Other Gene Editing Technologies
| Technology | Precision | Efficiency | Complexity | Applications |
|---|---|---|---|---|
| CRISPR-Cas9 | High | High | Relatively simple | Wide range, including genetic diseases, cancer, and agriculture[1][2][3] |
| ZFNs (Zinc-Finger Nucleases) | High | Moderate | Complex and labor-intensive | Limited to specific applications due to design complexity[3] |
| TALENs (Transcription Activator-Like Effector Nucleases) | High | Moderate | Complex and labor-intensive | Limited to specific applications due to design complexity[3] |
| CRISPR-Cpf1 | High | High | Simple | Offers greater control over target DNA sequences, especially useful in certain instances[1] |
Detailed Bullet Point List: Ethical Considerations in Using CRISPR
-
Germline Editing:
-
Permanent changes to the human genome
-
Potential for creating “designer babies”
-
Unequal access to the technology
-
Unintended genetic errors affecting future generations[1][2][4]
-
Off-Target Effects:
-
Risk of unintended mutations
-
Potential for serious health consequences
-
Need for improved precision and safety measures[3]
-
Access and Equity:
-
High cost of CRISPR-based therapies
-
Limited accessibility to certain populations
-
Need for equitable distribution of benefits[1]
-
Public Perception and Regulation:
-
Need for clear regulatory frameworks
-
Importance of public education and engagement
-
Global consensus on ethical use[2][5]
-
Balancing Benefits and Risks:
-
Weighing therapeutic benefits against potential risks
-
Continuous research to improve precision and safety
-
Transparent and rigorous clinical trials[1][2][3]
Quotes from Key Figures
- Jennifer Doudna: “We must always be careful and responsible when dealing with such impactful technologies. Imagine, for example, if we had the power to engineer ‘improved humans’ with specific traits and capabilities or to efficiently engineer many of the animals and plants around us. We might dramatically change the course of evolution.”[2]
- Emmanuelle Charpentier: “Following the birth of gene-edited babies, some medical and bioethics researchers, including myself, called for a moratorium on editing human genes in eggs, sperm, or embryos. We contend that because there remain many unknowns about the technology, scientists may unintentionally introduce as many genetic errors as they attempt to fix.”[1]
As we navigate the complex landscape of CRISPR technology, it is essential to approach these ethical dilemmas with caution, responsibility, and a commitment to ensuring that this powerful tool benefits humanity while minimizing its risks.